My 88-year-old mom, who fell and broke her arm some eight weeks ago, had to endure a two-pronged battle – with herself and with the health care system.
I suspect that her story, while not tragic, is more commonplace than generally recognized. But, as with other common experiences, it carried the potential for tragedy.
After less than a week in the hospital, she was sent home with her arm in a sling. No need for surgery. It was a clean break, the arm would heal on its own.
In her bed at my sister’s home, where she’s lived since her stroke more than four years ago, things went from bad to worse, and not just for my mom.
It was a nightmarish week for my sister, who had to get up three or four times in the middle of the night to help our mother: give her the pain medication at the prescribed intervals, get her out of bed, escort her to the bathroom, and then back to bed, readjust the pillows, and so on, and on…
I relieved my sister a couple of nights and rapidly joined her and the legions of other family members throughout the land turning into basket cases while caring for loved ones 24/7. Regular work attendance, family and social life – much less moments of reflection about the beauty in life – quickly go out the window.
On the seventh day, I heard my sister’s frantic voice through my sleep. stumbled out of bed and into the room next door. There I found my sister on her knees beside our mother, both of them on the floor by the bed. Mom was breathing, snoring soundly, slouched over her good arm. “Should we put her back in bed? What if she’s injured something else? Her head, maybe? Should we call 911? Yes … no … yes.”
We opted for 911. In the ER later it was determined she had not injured any other part of her body. We surmised she must have rolled off the bed in her sleep, unconscious of what was transpiring. “Phew! That was a close one.”
There was a silver lining in all this. It took a second fall, soon after the first, to convince the insurance company that our mother needed extended professional care until the arm healed. No amount of logic or medical correctness had persuaded the insurer to approve extended care in a medical facility after the first fall.
After several days in the hospital, we lost the fight to place our mom in the acute rehab center where she had made satisfactory progress four years earlier after her stroke and after a subsequent hip replacement. This, after the professional personnel at the rehab facility had determined she was a prime candidate for their intensive program. We discovered later that the cost of care there was too high for the insurance carrier.
But we did take solace when we defeated efforts by the insurer to rush our mother instead into a dingy skilled nursing facility. We played low and dirty with the poor overworked social worker: “How would you like for your own mother to be placed in a dump?” After that and no small amount of persistent prodding at various levels of the health care bureaucracy, our mom was admitted into a decent skilled nursing facility.
A few days into her stay at the skilled nursing facility, my sister and I noticed our mother had intervals when what she said made little sense. We worried that she was beginning to lose it. We arranged to have the resident psychologist see mom during her weekly visits.
It wasn’t until several days later that it dawned on us to inquire about the pain medication. It turns out they were giving her a pill that contained morphine.
Morphine, commonly administered to patients in acute pain, sends my mother into a tizzy, including bouts of grouchiness and hallucination. So, the first thing out of our mouths any time our mom is transferred to a new health care facility is “Please, no morphine.” We are assured by the discharging facility that her chart so states.
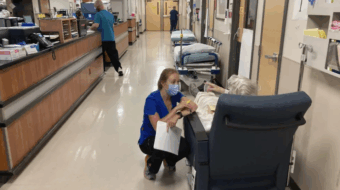
After four weeks at the skilled nursing facility, her arm was X-rayed. Things were healing nicely. Practically every day, my sister and her daughter, who has been a big help all along, pressed for an orthopedic doctor to examine our mom in order to determine whether she could start putting weight on her arm. The physical and occupational therapists were also pressing so they could start more aggressive treatment – the sooner that’s done, the quicker the recuperation.
It wasn’t until three weeks later – a day after our mom was discharged from the skilled nursing facility – that she was seen by an orthopedic doctor and certified capable of putting weight on the arm.
While at the skilled nursing facility, she regained her ability to walk on her own using a cane, for which we’re thankful. But save for some limited non-weight-bearing exercises, she received no therapy on the arm for which she was placed in the facility in the first place.
Neither protestations at the facility and with the insurance company nor the subsequent appeal to a supposedly impartial arbitrator changed the original decision to send my mom home on the day set by the insurer.
In the course of this experience, we’ve learned that under public Medicare it is the health care professional who has the final say on the best remedy, including how long it is necessary for a patient to remain in a medical facility. It is not a clerk or even a health care professional on the payroll of a for-profit outfit whose job depends on how well he/she satisfies the company’s profit line. Our family had initially opted for the private plan because it had a better prescription drug plan.
For folks our mother’s age, it is bad enough to have to endure the pain – physical and emotional – that comes with a serious injury. Not to mention the prolonged confinement in the health care facility. Judging from the comments of several patients our mother befriended, their ordeal felt more like incarceration. More than once staff members rushed out the facility’s front door to catch one patient who kept “escaping,” as the other patients would say, half jokingly.
Under the present for-private-profit-dominated health care system, inferior treatment and often life-threatening ordeals are heaped on patients who must already bear the crucible of their personal pain and fears.
I shudder to think what becomes of patients who don’t have family or friends to advocate for them.
Our mother is now recuperating at my niece’s home where there are no stairs to climb. It is with admiration that I watch the tender, patient and yet firm hand with which my niece cares for her grandma. My wife and daughter had taken shifts at the health care facility. In the process of fighting for our loved one’s welfare, the family has gotten closer and is more united than ever. As a result of this recent experience, our resolve to fight for health care reform has never been greater.
Deep inside, my heart cries out to do away now with this whole for-corporate-profit health care system and replace it with a democratically-run public system. But my better senses bring me back to reality. Let’s take care to pass the best health care plan present conditions will allow and, like Social Security and other social programs, improve on them with continued struggle.
Health care and a democratically-run system of public social benefits are on the horizon. Let’s keep our eyes on the prize.